What are the Best Treatments for Osteoarthritis?

Osteoarthritis or OA is a degenerative joint disorder (the most common type of arthritis) that is not curable but manageable with medication, surgeries, lifestyle changes and non-invasive treatments. Your doctor/physiotherapist diagnoses the condition after running specific tests and prescribes a treatment plan that would work best for you. So, the ‘best treatment for osteoarthritis’ rather depends on your individual medical history, severity of symptoms and preferences. This blog discusses the six most common osteoarthritis treatments recommended by medical professionals all over the world.
If you have been diagnosed with OA, life can be difficult, no matter what your age. But don’t lose hope. Science, research and technology have made it possible to manage osteoarthritis while navigating life steadily.
What are the Osteoarthritis Treatment Guidelines in Canada?
According to Arthritis.ca, osteoarthritis symptoms can be significantly relieved with self-management strategies and medications. Surgery is prescribed in severe cases only.
Here are the healthcare professionals allowed to treat osteoarthritis. They are registered to practice in their territory or province and have completed their training from a recognized university.
- A registered physiotherapist (PT)
- Occupational therapist(OT)
- Orthopedic Doctor
Another study outlined best practices for managing osteoarthritis (OA). Among these, three were developed in the United States, two originated from Europe, and one brought together international input from regions including Canada, Australia, China, Japan, and parts of Europe. Some guidelines also touch on surgical approaches, but the primary focus is on non-surgical, conservative management strategies.
Most recommendations are directed toward healthcare professionals, including physicians, physiotherapists, and other allied health specialists. Contributions from rheumatologists, general practitioners, orthopedic experts, physiotherapists, and sometimes rehabilitation, geriatric, sports medicine, and public health professionals helped shape these multidisciplinary guidelines.
Broadly, these approaches fall into four main areas:
- Education and Self-Management – Empowering individuals to understand their condition, manage symptoms, and take an active role in their recovery.
- Exercise and Weight Management – Promoting regular movement and maintaining a healthy weight to reduce pressure on joints and improve function.
- Joint Support and Assistive Devices – Using braces, walking aids, or supportive tools to enhance stability and ease daily activities.
- Complementary and Alternative Therapies – Incorporating evidence-backed practices such as acupuncture, massage, or mindfulness to support pain relief and overall well-being.
Together, these strategies emphasize a comprehensive, patient-centered approach, one that combines movement, education, and lifestyle changes to improve joint health and quality of life.
What are the Effective treatments for Osteoarthritis?
There is a protective cartilage on the ends of your bones. It acts as a shock absorber and lubricator, allowing the joints to move freely. In osteoarthritis, this cartilage wears down due to age or injury, causing the bones to rub against each other during movement. The condition causes pain and stiffness in the joints of the hands, knees, lower back and neck. It makes everyday movements like walking, bending, or gripping harder than before. So, the treatments focus on reducing pain and restoring optimum joint movement.
Exercise/Physical Therapy
Exercises, when done with the right form and under professional supervision, help manage osteoarthritis over the long term. The modern treatment model for OA prioritizes exercise and lifestyle changes, which leads to long-term health and function rather than just masking
the symptoms. Physical therapy causes a complex interplay of biomechanical, biological and immunomodulatory mechanisms within the body, relieving OA symptoms significantly.
How Do Exercises Help Manage Osteoarthritis Symptoms?
Stronger muscles- Strong muscles are critical to joint stability. Thus, exercises focus on strengthening the muscles around the affected joint. As the muscles regain their strength, they also resume their function as a dynamic, responsive “brace” that protects the joint. Studies have demonstrated a clear link between weaker quadriceps strength and an increased risk of developing knee OA, particularly in women, suggesting that strength training may play a preventative role.
Smooth Joint Movement- Movement promotes circulation of synovial fluid and nutrient exchange in the joint. This helps maintain cartilage health and reduces stiffness.
Better Neuromuscular Control- Exercises improve proprioception (the sense of joint position), balance, and coordination. This is crucial for individuals with OA, as it improves the body’s ability to stabilize joints during dynamic activities, reducing the risk of flare-ups.
Lower Inflammation- As little as 20 minutes of moderate physical activity has been shown to produce a measurable anti-inflammatory cellular response. Research shows that regular activity is associated with reduced local and systemic inflammatory markers and improved pain modulation by the nervous system.
Overall, physical therapy plays an active role in osteoarthritis pain relief and overcoming movement challenges. Your physical therapist prescribes exercises based on your recovery needs.
Common Exercises Recommended
|
Type of Exercise |
Purpose | Examples |
Recommended Frequency |
| Strengthening (Resistance) Exercises | Increase muscle strength and joint stability. | Squats or sit-to-stand progressions, straight-leg raises, resisted hip abduction. | 2–3 times per week with gradual progression. |
| Low-Impact Aerobic Exercises | Improve cardiovascular fitness, aid weight control, and reduce pain with minimal joint stress. | Walking, cycling, swimming, using an elliptical. | Most days of the week at moderate intensity. |
| Range-of-Motion & Flexibility Exercises | Maintain or improve joint mobility and reduce stiffness. | Gentle knee/hip flexion–extension, calf/hamstring stretches, yoga stretches for mobility. | Short daily sessions are helpful. |
| Balance & Proprioception Exercises | Improve coordination, reduce fall risk, and support joint control. | Single-leg stands (with support as needed), tandem stance, heel-to-toe walking. | A few times per week, especially for older adults. |
Conservative Therapies
Conservative treatments relieve osteoarthritis pain through non-invasive techniques and lifestyle modifications. They are usually the first line of treatment for osteoarthritis, with a focus on relieving pain, improving function, and delaying disease progression. The following are the two most effective conservative treatments for OA.
Physiotherapy
Evidence indicates that physiotherapy treatments should be initiated at the time of diagnosis and implemented either before or simultaneously with pharmacological treatments. While exercise is a crucial part of physiotherapy programs, patients may be recommended other modalities too, depending on their individual needs.
Common Physiotherapy Treatments for Osteoarthritis
|
Technique |
Purpose |
Examples |
| Manual Therapy | These skilled, hands-on techniques primarily focus on reducing joint stiffness and improving range of motion. | Gentle joint mobilizations, soft tissue massage. |
| Therapeutic Exercise | Exercises reduce pain and improve function in OA patients. While strengthening exercises improve the muscles to support and offload the joint, aerobic exercises lead to anti-inflammatory effects. | Strength training, stretching, and low-impact aerobics. |
| Patient Education | Physiotherapists empower OA patients with the knowledge, skills, and confidence to manage their own condition for the long term. | Home exercise plans, joint protection tips, ergonomic advice and pain management strategies. |
Physiotherapy programs are highly individualized. It is unique to every patient, catering to their unique needs. If joint pain has been troubling you, especially in the hands, feet or knees, get it assessed by a licensed physiotherapist. They can diagnose the condition and guide you through a safe, progressive plan to stay active with confidence.
Occupational Therapy
Occupational therapy helps OA patients live full and productive despite the challenges of this condition. The licensed therapist assesses your symptoms and creates a personalized plan to reduce your pain and restore your ability to do daily activities at home or work.
Main Goals of Occupational Therapy in OA Management
Pain and symptom management- Occupational therapists (OTs) address pain and stiffness with non-pharmacological methods.
Joint protection- OTs guide you through techniques to protect the affected joint from further damage and to conserve energy.
Adaptive training- The experts train you to use adaptive equipment that can make daily tasks easier and less painful with OA.
What Are the Techniques OTs Use to Treat OA?
|
Technique |
How It Helps |
Examples |
| Joint Protection Strategies | Encourages use of stronger joints and better movement patterns to minimize strain on affected areas. | Using the shoulder instead of fingers to lift items, carrying objects close to the body, avoiding tight grips, and using two hands instead of one. |
| Activity Modification | Adjusts how activities are done to avoid positions or motions that worsen symptoms. | Using adaptive tools for cooking, sitting while performing chores, and reorganizing workspaces to reduce reaching or bending. |
| Assistive Devices & Adaptive Equipment | Reduces physical effort and joint load during daily activities. | Jar openers, button hooks, reachers, long-handled sponges, raised toilet seats, ergonomic kitchen tools. |
| Energy Conservation Techniques | Helps individuals plan and pace tasks to avoid overexertion. | Breaking tasks into smaller steps, alternating heavy and light tasks, and resting before fatigue sets in. |
| Splinting and Orthotic Support | Limits painful joint movement and supports function. | Hand or wrist splints, thumb braces, and knee supports for joint alignment during tasks. |
| Pain Management Education | Empowers self-management through awareness and behavioural changes. | Teaching heat/cold application, relaxation techniques, proper posture, and pacing. |
| Environmental & Ergonomic Modifications | Prevents joint strain and improves accessibility. | Adjusting desk height, using cushioned grips, and rearranging storage to minimize bending/reaching. |
| Psychosocial Support & Coping Strategies | Builds confidence and reduces frustration or depression related to limitations. | Teaching stress management, goal-setting, and promoting engagement in enjoyable activities. |
Medications
Your doctor may recommend medications when foundational treatments aren’t enough to control pain. Consult with your healthcare provider to know the right prescription medicines for your recovery.
The medications usually include:
|
Treatment Type |
Use |
Key Notes |
| 1. Topical Treatments (Creams and Gels) | Recommended for joints close to the skin, such as the hands and knees. These medications provide localized pain relief with a lower risk of systemic side effects compared to oral drugs. | Ideal as a first-line option for mild to moderate, surface-level joint pain. Apply as directed and avoid contact with eyes or broken skin. |
| 2. Oral Medications | Used when topical treatments are insufficient. Help manage systemic pain and inflammation, but require caution due to potential side effects. | Discuss dosage and duration with a healthcare provider. Long-term NSAID use may cause stomach, kidney, or heart-related side effects. |
| 3. Injections for Targeted Relief | Used for more severe or persistent symptoms when other treatments are not enough. Provide localized, temporary relief. | Results vary; not always covered by health plans. Injections should be performed by qualified healthcare professionals. |
Surgery
Surgery is generally the last resort to control OA when all other treatments fail. Hip and knee replacements are among the most effective surgeries performed in Canada.
What are the Alternative Treatments for Osteoarthritis(OA)?
Osteoarthritis treatment isn’t restricted to physiotherapy, though the latter is an integral part. Effective management of OA involves a variety of conservative and adjunctive therapies that support overall joint health and function. The following approaches, along with non-invasive treatments, contribute uniquely to long-term relief from OA pain.
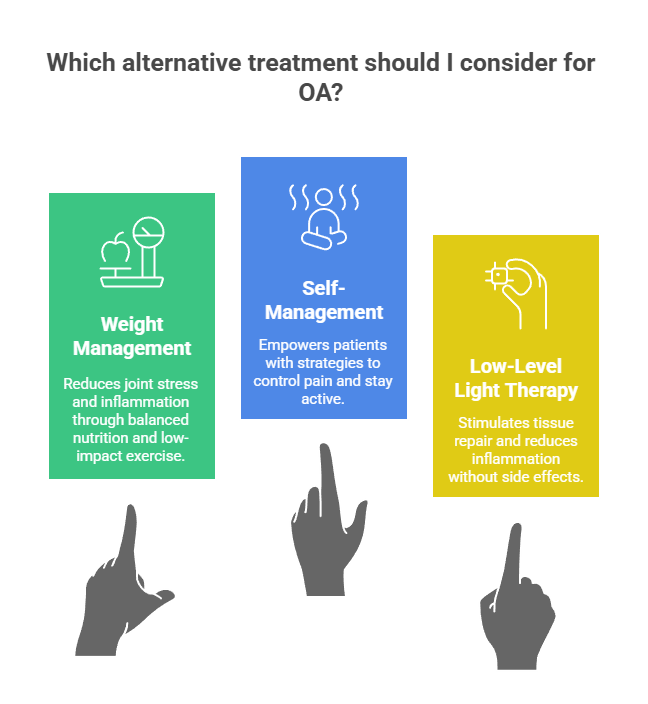
Weight Management
Maintaining a healthy body weight plays a pivotal role in managing osteoarthritis, particularly in the knees, hips, and lower back. Every extra kilogram of body weight adds roughly four kilograms of pressure on the knees during movement. It is recommended to shed 5-10% of body weight to significantly reduce joint stress, pain and stiffness. Weight management also reduces the inflammatory response associated with OA.
A combination of balanced nutrition and regular low-impact exercise, such as swimming, cycling, or walking, is most effective. This dual approach helps maintain muscle mass while supporting joint function. Research from the Osteoarthritis Research Society International (OARSI) highlights weight control as one of the most powerful non-pharmacologic interventions to slow disease progression and enhance quality of life.
Self-management
Learning to take care of osteoarthritis on your own helps people feel more in control of their joint health and daily life. Physiotherapists can help you understand what triggers the pain, how to pace activities and when to rest. In other words, they empower with impactful lifestyle habits that act as the key to long-term success.
A few effective self-management strategies
- Stay physically active with low-impact exercises.
- Follow a balanced diet to maintain a healthy weight.
- Alternate activities with rest using the “20–20 rule”: after 20 minutes of activity, rest or stretch for 20 seconds.
- Use a warm compress in the morning for stiffness, and a cold pack after activity to reduce swelling.
- Work closely with your physiotherapist, occupational therapist, or physician.
Cognitive-behavioural approaches are also effective in reducing anxiety and depression linked to chronic pain. Self-management programs led by physiotherapists, occupational therapists, or arthritis foundations teach participants how to adapt daily routines safely and stay active despite discomfort. Self-management is considered a foundational component of OA care, equally as important as exercise. It shifts the focus from treatment dependency to self-efficacy.
Low-level light therapy (LLLT)
Low-Level Laser Therapy (LLLT), also known as cold laser therapy, is a non-invasive technique that uses light wavelengths to stimulate tissue repair, enhance circulation, and reduce inflammation. The therapy works at a cellular level by improving energy production in mitochondria, which helps reduce pain and promote healing in damaged tissues.
In osteoarthritis, LLLT is particularly beneficial for the areas prone to stiffness and swelling, such as the knees, hands, and shoulders. According to several studies, consistent laser therapy sessions can decrease pain intensity, improve joint mobility, and complement exercise-based rehabilitation. Unlike medications, LLLT has no systemic side effects, making it suitable for long-term symptom control. According to emerging evidence, combining LLLT with physiotherapy or strengthening exercises yields the best outcomes. As an evolving therapy, it holds promise for patients looking for a gentle yet effective adjunct to traditional osteoarthritis management.
Conclusion
Osteoarthritis is a common arthritis that affects at least 1 in every 10 Canadians. There is no cure for this condition, but you can learn to manage the symptoms and lead an active life despite the challenges. Personalized exercise programs form the foundation of OA care and rehabilitation with strengthening, low-impact aerobic work, flexibility and balance training exercises. Physiotherapy is considered one of the most effective non-surgical treatments for osteoarthritis. The physiotherapist helps reduce pain, improve joint mobility, restore function, and enhance quality of life through personalized movement-based therapy.
At the same time, conservative and adjunctive therapies such as acupuncture, low-level laser therapy (LLLT), and self-management programs offer additional layers of relief and empowerment. Together, they create a holistic system that targets pain from multiple angles while promoting long-term joint health.
Ultimately, managing OA is about progress, not perfection. Small, consistent efforts guided by professionals can lead to meaningful improvements in comfort, confidence, and quality of life. With an active mindset and a personalized care plan, living well with osteoarthritis is absolutely possible.
Blog Categories
- Acupuncture Treatment (10)
- Ankle Sprain (1)
- Arthritis Treatment (1)
- Back Pain (23)
- carpal tunnel (2)
- Chiropractic Care (39)
- Tennis Elbow (1)
- Chronic Pain (7)
- COVID-19 (1)
- Custom Orthotics (6)
- Dizziness (4)
- Exercises (13)
- Foot Orthotics (6)
- Hamstring Stretches (2)
- Info Articles (3)
- Kids Injury (1)
- Laser Therapy (4)
- Massage Therapy (21)
- Neck Pain (17)
- Orthopedic (1)
- Osteoarthritis (5)
- Osteopathy (3)
- Pain Management (21)
- Physiotherapy Benefits (44)
- Physiotherapy Clinic (6)
- Physiotherapy Exercises (12)
- Physiotherapy Tips (25)
- Physiotherapy Treatment (101)
- Rotator Cuff (2)
- Shin Splints (1)
- Shoulder (2)
- Spine (4)
- Sports Physiotherapy (2)
- Uncategorized (1)
- Vestibular Physiotherapy (2)
- Work From Home (2)